
New Research Challenges How We Treat BV—Here’s What You Should Know
For decades, bacterial vaginosis (BV) has been treated as a frustrating, recurrent condition that affects only women. It impacts nearly one in three women of reproductive age and is linked to serious health consequences, including an increased risk of STIs, pelvic inflammatory disease, and preterm birth. Yet despite its prevalence and the fact that 60% of cases recur within a year, treatment guidelines have failed to acknowledge an essential factor: the role of male partners in transmission.
Now, a landmark study published in The New England Journal of Medicine (NEJM) may finally change the way BV is treated. The study provides strong evidence that BV is sexually transmitted and that treating male partners dramatically reduces recurrence in women—confirming what many researchers have long suspected.
The study that changes everything
This randomized, controlled trial—led by Dr. Lenka Vodstrcil and her team in Australia—tracked 164 monogamous couples in which the female partner had BV. The couples were divided into two groups:
- Control group: Women were treated with standard oral or vaginal antibiotics, while their male partners received no treatment.
- Partner-treatment group: Women received the same antibiotics, but their male partners were also treated with a 7-day course of oral metronidazole and a topical clindamycin cream applied to the penis.
The results were so striking that an independent safety board stopped the trial early to allow all participants access to the treatment.
- 63% of women in the control group (who were treated alone) experienced recurrence within 12 weeks.
- In contrast, only 35% of women in the partner-treatment group had BV return—a nearly 50% reduction in recurrence.
This paradigm-shifting finding suggests that male partners harbor and reinfect their female partners with BV-associated bacteria, and that previous treatment strategies have ignored a critical piece of the puzzle.
Why did previous studies miss the mark?
This isn’t the first time researchers have tried treating male partners to prevent BV recurrence—but earlier studies failed to show a benefit. Those failures led many medical experts to dismiss the idea that BV was sexually transmitted. However, those studies had flaws:
- They only used oral antibiotics for men, which failed to address the BV bacteria that persist on the penile skin.
- They did not ensure treatment adherence, meaning some participants may not have taken the full course of medication.
- They lacked statistical power, making it hard to detect meaningful differences.
By adding a topical antibiotic cream to treat bacteria on the penile skin, this new study finally produced conclusive evidence that treating both partners works.

The bigger picture: BV as an STI
BV has long been excluded from the STI category, but this study adds to growing evidence that it should be reconsidered. BV-associated bacteria have been found in the male urethra and on penile skin, and women with regular sexual partners have double the risk of recurrence compared to those without. The penile microbiome itself may even predict a woman’s risk of BV, reinforcing that BV is not just a vaginal issue—it’s a shared bacterial ecosystem.
With these findings, medical guidelines may finally shift, just as they did for HPV and Mycoplasma genitalium. As Dr. Christina Muzny put it, “It’s time for men to take shared responsibility for treating this infection.”
What does this mean for women's health?
For too long, BV has been treated as a chronic, frustrating condition rather than an infection with a clear transmission pathway. This study could finally change that, leading to better treatment guidelines, improved diagnostic tests, and a shift in how BV is understood.
Still, questions remain. Some women continue to experience recurrence even without sexual activity post-treatment. Researchers believe that certain strains of BV-associated bacteria may be more resistant to antibiotics, or that immune and hormonal factors could play a role. Understanding these mechanisms will be key to truly solving BV.
How is Evvy leading the way?
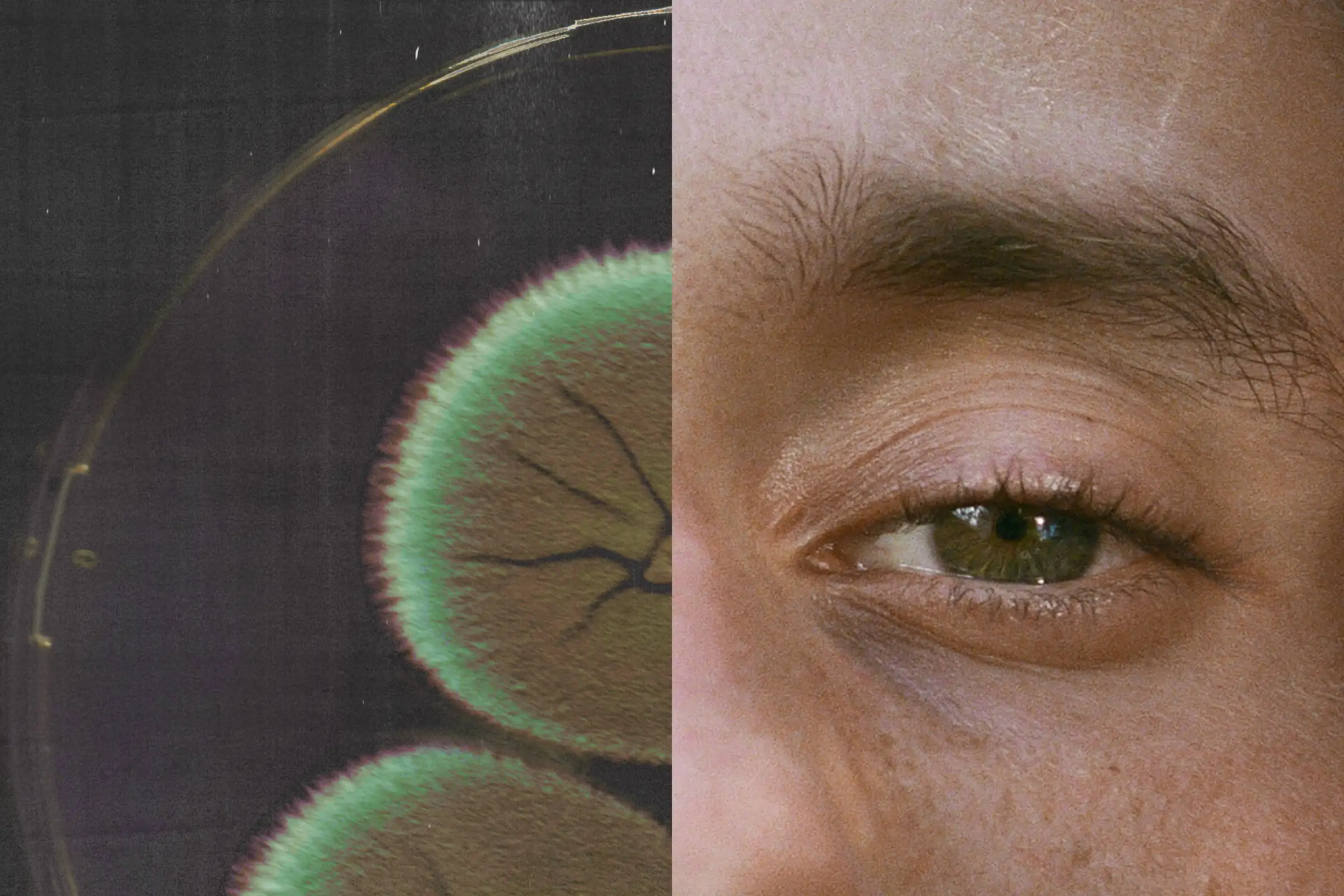
At Evvy, we’ve always believed BV is more than just a nuisance—it’s a serious but solvable health issue. That’s why we’re pioneering precision vaginal healthcare through metagenomic sequencing, which allows us to identify all bacteria and fungi in the vaginal microbiome with unprecedented accuracy.
This research only strengthens the case for a more advanced, science-backed approach to BV care. By leveraging our technology and real-world patient data, Evvy is working toward better diagnostic tools, targeted treatments, and a future where BV is no longer a cycle of frustration but a condition with clear, effective solutions.






