
Vaginal Microbiome and Fertility: How Are They Linked?
Learn more about the link between the vaginal microbiome and fertility, and whether a healthy vaginal microbiome can affect pregnancy outcomes.
Words by Dr. Krystal Thomas-White, PhD
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Christine Vo, MD
Deciding to have a baby is a big, emotional, life-changing decision. So if you are somewhere on your fertility journey, know that we see you and know that you are going through a lot!
If you are like many people, you spent the majority of your reproductive life up till this point trying not to get pregnant. And now that you decided to have a baby you are ready to get pregnant. This is an exciting time, but also realize that these things take time and that the unknown can feel scary and overwhelming. That’s why throughout this process, information and education can be your best friend.
Below, we walk you through fertility, infertility and its causes, and their relationship to the vaginal microbiome.
When should I be concerned about my fertility?
If you are under 35, it’s recommended that you try to conceive naturally for at least one year before turning to fertility treatments such as in vitro fertilization (IVF). In that time 85% of couples will conceive naturally. If you're older than 35, your doctor might recommend decreasing this window to six months or less.
There are lots of things you can do to increase your chances of conceiving in this first year.
- Stay healthy: Get regular exercise, eat healthy, get plenty of rest, stop smoking, and cut back on alcohol.
- Prenatal visits: Be sure to schedule a preconception health care visit to talk over your plans with your doctor. During this appointment your doctor will talk to you about getting off birth control, what to expect with your cycle, and when to check back in.
- Prenatal vitamins: Start your prenatal vitamins as soon as you start trying. Proper levels of folic acid (found in all prenatal vitamins) prevent birth defects that can arise in the first few weeks of pregnancy. So it is important to start taking these vitamins before you even know you are pregnant.
- Cycle tracking: There are numerous apps on the market to help you figure out when your fertile window is. But the most accurate ones take into account a spike in your luteinizing hormone (LH). This hormone is responsible for initiating ovulation, and is the primary signal that your fertile window has begun.
- Vaginal microbiome testing: Research shows that the composition of the vaginal microbiome can impact conception, implantation, and pregnancy outcomes. Understanding your vaginal microbiome—and whether it’s in an optimal state for fertility—can provide insights before trying to conceive.
Each individual and couple is unique and has a unique set of considerations. LGBTQ+ couples or individuals conceiving on their own have specific challenges, like egg or sperm donation, or surrogacy to consider that we are not covering here. If this is you, we recommend talking to a fertility specialist or one that specializes in LGBTQ+ couples.
A note on miscarriages
A miscarriage is the spontaneous loss of pregnancy before 20 weeks gestation and the majority happen in the first trimester. In fact, many women might have a miscarriage before they even know they're pregnant. About 10-20% of pregnancies end in miscarriage. The Centers for Disease Control and Prevention (CDC) estimates that about half of women will experience at least one miscarriage in their lifetime.
Miscarriages can be emotionally devastating but know that they are never your fault. Most miscarriages are the result of your body identifying that the fetus is not developing properly, maybe due to something like a chromosomal abnormality. It’s your body’s way of identifying that the fetus would not have developed into a healthy baby. It’s important to know that miscarriages are one-off events and most people go on to have a healthy baby in their next pregnancy.
So let’s say that you have done all the above and now you are wondering if you should go get your fertility checked. What does that look like?
Assessing fertility and causes of infertility
Female fertility, like much of women’s health, is poorly understood and is affected by many different factors. Talking to a fertility specialist will start you on the right track.
It’s also important to mention that fertility is not just the responsibility of the person with a uterus as there are multiple male-factor fertility challenges that can arise. The world health organization (WHO) estimates that 40-50% of infertility is attributed to “male factor” infertility. Again, talking to a fertility specialist will help figure out where to start.
In general there are multiple categories of female infertility including:
- ovulation disorders
- uterine abnormalities
- tubal obstruction
- peritoneal factors
- potential cervical factors
- immunological factors
- unexplained infertility.
Your fertility specialist will run a variety of tests to figure out if you fall into any of the above categories.
Types of infertility
Ovulation disorders
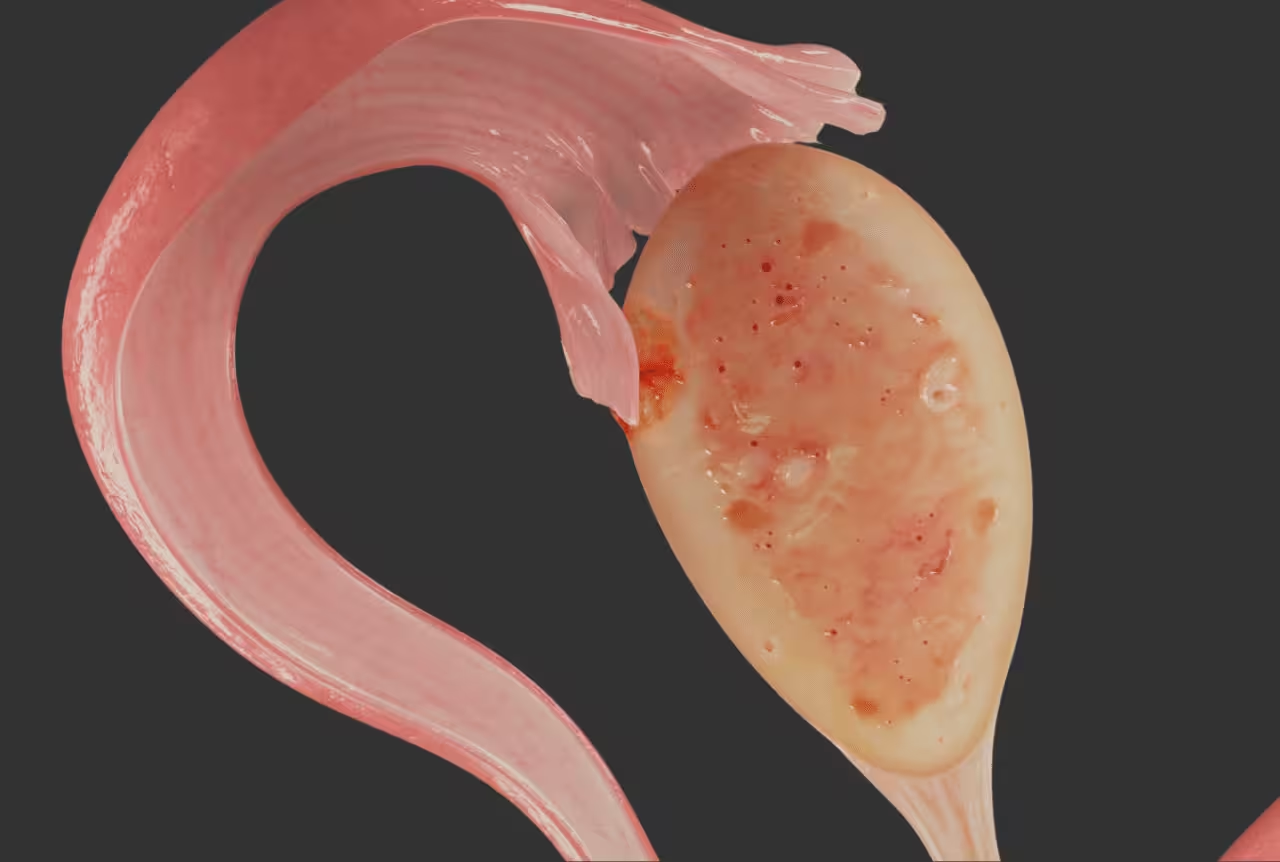
Ovulation, or the release of an egg from the ovary, is a complex process aided by an array of different hormones.
The WHO separates this category into three groups:
- hypothalamic-pituitary failure
- dysfunction of the hypothalamic-pituitary-ovarian axis
- ovarian failure.
Some causes for these different categories include low or high body weight or hormonal conditions like polycystic ovary syndrome (PCOS). To diagnose this, your doctor will test your hormones and assess ovulation.
Tubal obstruction
The fallopian tubes are the thin tubes that connect your ovaries to the uterus and are required for delivering the egg to the uterus for successful implantation and pregnancy. There can sometimes be an obstruction in the tubes that prevents healthy eggs from getting to the uterus, this is called a tubal obstruction. Tubal obstructions can occur for a variety of reasons, from endometriosis adhesions, pelvic inflammatory disease (PID), previous surgeries, or even ectopic pregnancies. Your doctor may do an imaging test to look for patent fallopian tubes.
What is the connection between the vaginal microbiome and fertility?
It’s complicated, but science is actively trying to figure out if there is a link between the reproductive tract microbiome and fertility.
In general, multiple studies show that a healthy vaginal microbiome (dominated by Lactobacillus species) is beneficial for fertility, while vaginal dysbiosis is associated with infertility. Remember this isn't a hard and fast rule, but just an association. Many of the studies vary based on what microbiome they are measuring (cervical, vaginal and endometrial microbiome) or what population of people (healthy preconception, or those undergoing assisted reproductive technologies like IUI and IVF).
One thing we do know for sure is that bacterial vaginosis (BV) is associated with higher risk of sexually transmitted infections (STIs), and STIs are associated with an increased risk of pelvic inflammatory disease (PID) which can lead to future fertility problems. So if you’re sexually active, be sure to get regular STI tests.
So how do you know if your vaginal microbiome is optimized for conception? Evvy’s Vaginal Health Test offers Fertility Insights to help provide a clearer picture of your fertility by analyzing four biomarkers:
- Protective Score– Measures the beneficial bacteria that create an optimal environment for sperm survival.
- Microbiome Diversity Score– Assesses bacterial balance linked to implantation and pregnancy success.
- Fertility Disruptors– Detects microbes associated with inflammation and conditions like BV.
- STI Status– Screens for infections that can interfere with conception and pregnancy.
By analyzing these markers, Evvy helps individuals understand whether their vaginal microbiome may be supporting or disrupting their fertility—offering actionable, science-backed next steps to optimize their microbiome health.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
The vaginal microbiome and time to natural conception
One study in 2022 correlated the vaginal microbiome and the time it took for 89 women to get pregnant. They found that 59.6% of women became pregnant within a year, and Lactobacillus was higher in the women who became pregnant, and Gardnerella (a bacteria linked to bacterial vaginosis) was higher in women who did not get pregnant.
The vaginal microbiome and assisted reproductive technology
A recent meta analysis of 17 studies, which included 3,543 patients, found that vaginal dysbiosis in vitro fertilization (IVF) couples was associated both with early pregnancy loss as well as a reduction in clinical pregnancy rate.
However, it’s unclear what specific role the vaginal microbiome is playing in fertility compared to other upper reproductive tract microbiota (like the cervical or uterine microbiome). It’s also unclear how comparable these three microbial niches are to each other. Additionally, the endometrium is a lower biomass niche and is harder to sample — most of the time a biopsy is needed.
Male seminal microbiomes and fertility
Finally, the male seminal microbiome might also play a role. Semen has its own microbiome and some studies suggest that the seminal microbiome can affect fertility. Or that the interaction between the vaginal microbiome and semen might be a factor. For example, research suggests that the vaginal microbiome might actually affect whether or not sperm is successful at reaching the egg.
Immunological factors
The vagina microbiome can affect your immune system, and immunology plays a huge role in pregnancy outcomes.
Sperm, the embryo, and the fetus are all foreign bodies to the maternal host and her immune system is constantly striking a balance between allowing the fetus to grow and protecting the host from this foreign entity. Weird to think of it that way, but it’s true!
This particular area of research is very new, but here are a few high level ideas around the connection between the vaginal microbiome and pregnancy outcomes:
- Hormones and immunology are tightly linked. And hormones and the microbiome are also interconnected. Changes in sex hormones and other hormones (thyroid, pancreas, or even insulin) can alter the vaginal microbiome as well as the immune system which could make it easier or harder to develop a successful pregnancy.
- Implantation of the embryo into the uterus is accompanied by an inflammatory response. It’s hypothesized that simply the act of taking a biopsy can improve fertility rates because it primes the uterus for the immune state needed for implantation.
- The maternal-fetal interface may improve the anti-inflammatory state needed for the second trimester.
We know that there are so many things to consider (and try) when experiencing infertility. Though the research on the relationship between the vaginal microbiome and fertility is still emerging, taking a vaginal microbiome test like Evvy’s can help you get a clear and comprehensive picture of the composition of the vaginal microbiome.
If you find out you have high levels of disruptive bacteria in your vaginal microbiome (like Gardnerella), you can have a conversation with your healthcare provider on how to shift your vaginal microbiome to a more protected state that may support your chances of conceiving.
As we said before, when it comes to your fertility journey, the more information you have about your body and vaginal health, the better.




.avif)
.avif)