SheMD Podcast: Priyanka Jain on the Future of Women's Health and the Vaginal Microbiome
Priyanka Jain, co-founder and CEO of Evvy, recently sat down with the SheMD podcast for a thought-provoking discussion about the future of women’s health.
The SheMD podcast is a platform dedicated to empowering and supporting women in medicine, where real-life experiences and candid conversations take center stage. Hosted by Mary Alice Haney and OBGYN-to-the-stars Dr. Thais Aliabdi, SheMD dives into the challenges and triumphs faced by women in the medical field. Together, they create an engaging space that highlights the voices of female medical leaders, discusses pertinent issues, and promotes a culture of support and solidarity.
In this episode, Priyanka talks about all things vaginal health, the need to destigmatize discussions around women’s health, and how Evvy is empowering women to better understand their bodies. Together with Dr. Aliabadi, she also offers practical tips for maintaining a healthy vaginal microbiome — including the importance of monitoring changes, being mindful of antibiotic use, and staying proactive about testing when necessary.
This episode is a must-listen for anyone curious about the intersection of innovation and personalized healthcare for women.
Watch the full episode and read the transcript below to learn more about Priyanka's journey, the evolving landscape of women's health, and Evvy’s mission to empower women through better healthcare solutions.
Mary Alice Haney: On today's podcast, we have Priyanka Jain, who is the founder of Evvy. And I am so excited to have this conversation with you because I want to start off the whole thing by just: saying vagina, vagina, vagina.
Dr. Thais Aliabadi: Here we go! Story of my life.
Mary Alice: Vagina, vagina, vagina, vagina, vagina, vagina. I'm so happy that people are actually to start talking about the vagina, they're talking about menopause, we're talking about PCOS. All of these conversations are happening. Dr. A and I were at the Fortune Women's Health event and we met your incredible father, who is also an entrepreneur (he started Viome). This is a family of geniuses and you know, you're changing access and what we do on this podcast, and the reason that Dr. A wanted to start it, was to take all the information we have and put it in the hands of women at home. And that's exactly what you're doing at Evvy. So will you give us the whole story?
Priyanka Jain: Absolutely. Well, first, I have to say thank you so much, one, obviously for having me, but two, for the amazing work that you're doing. I mean, guess who the people are who are destigmatizing all of these conditions: It's people like you who are using your platform, and your amazing expertise to make these conditions not so stigmatized for so many women around the country and the world. So truly so grateful for the work that you both are doing. And excited to talk about Evvy today, and to talk about the vaginal microbiome. Have you guys talked about the vaginal microbiome yet?
Dr. A: Nope
Mary Alice: First time, first time.
Priyanka: I'm honored.
Dr. A: Can you tell us more about yourself, your education, what your major was? I just want to know a little bit more about your background.
Priyanka: When I was younger I worked a lot in nonprofits for women around the world. I worked with the UN Foundation on the Girl Up campaign. I was working on building a school in Afghanistan for girls. And I really was a strong believer that there were so much opportunity in so many girls around the world that was untapped because women simply didn't have access to the same education, healthcare, leadership, tools to enable them to succeed.
When I went to Stanford, it was the first time that I saw the power of science and technology to scale the impact that we were having in more of a nonprofit context. And that if we could actually give women access to better science to better technology, we could radically accelerate our ability to increase opportunity for women. When I was at Stanford the degree I did was called “Science, Technology and Society”. I always laugh because what is not science, technology, or society? I don't know. But essentially you do kind of a core of computer science, electrical engineering, mechanical engineering, and then you also do a variety of classes across the business school and the design school. So really trying to understand how are solutions built, and then how do you think about problems that people are facing and the best way to design solutions for that?
I came out of college to join a startup and moved out here to New York and joined an amazing company that was building algorithms to try to make the hiring process more fair. As we all know, looking at where we went to school and what our GPAs were are not the best predictors of our success. And there's an amazing woman who had started this company. She was a PhD neuroscientist who wanted to bring her neuroscience research to the hiring process and so spent almost five years really helping build that company. I was the Head of Product there and oversaw a lot of really interesting data science, machine learning challenges, but also human challenges, how do you convince people to change their biases around human potential? Back in 2015, it was kind of before the current age of AI, if you will, and so much of what we were working on was when you have biased data sets, how do you actually build fair algorithms? If currently, high-performing investment bankers are primarily white men named John, how do you build an algorithm that performs successfully on the people like the three of us?
And I also never could have imagined how much overlap there was between kind of the challenges that exist in HR, if you will, around what is the data that we've decided is important? How are we storing it? How are we building technological tools on top of it? And then what we see in healthcare. So I saw an opportunity when I realized the data gap, to really leverage my background from the data side to help solve a set of problems in women's health.
People always ask me, how in the world did you end up starting a vaginal microbiome company? Because I guess everyone else does not wake up thinking about the vaginal microbiome. And at the same time had been dealing with so many quote-unquote, kind of mysterious health issues. Experiencing all of the symptoms that Dr. A you probably see all the time and felt like no matter which specialist I went to, which doctor I went to, I was constantly being told to drink more water, and maybe I needed to sleep more, and maybe I had too stressful of a job. And I just couldn't believe that in my day job, I was sitting there thinking, we can measure anything, we can predict anything in the world. And then I was like, wow, well, I guess if it has to do with my female body, the hands go up, and we don't have the tools to really help women understand what's going on and how they can fix it.
As I did some of my own research, which I think so many women end up doing, that was when I found out that women weren't required or really allowed in clinical research in the U.S. until 1993, which made my entire life make sense. I also learned that women are to this day diagnosed on average four years later than men across over 770 diseases. And at that moment, I was like, wow, there's actually a massive data gap when it comes to our understanding of the female body.
And there's this huge opportunity for us to actually start to do the basic science, to do the basic research, to build the data sets on the female body so that we could actually predict risk of disease or diagnose disease or treat disease as it uniquely manifests in half of the population. And so our focus at Evvy is really on what are those overlooked biomarkers or just those signals that the female body is constantly giving off to try to tell us where things are going right and where we need help. But we're just not measuring those things today because, frankly, we only ever studied middle-aged, mid-sized white men.
Dr. A: No, it's true!
Mary Alice: No, it's honestly true. Did you know that early statin trials were studied on men, even though heart disease is still the leading cause of death in women?
Priyanka: It's mind-blowing. I think it was actually only in 2016 that we required female mice in research. So we have a long ways to go in our understanding of the female body. And obviously at Evvy, our first focus is on the vaginal microbiome, which does not get talked about enough given the role that it's playing in our lives.
Mary Alice: Amazing. That's incredible. Let’s start at the core level. There's been so much about the gut microbiome, how it's affecting your mental health, all of that. So, talk about the vagina. Talk about the vagina.
Priyanka: I mean, I think Dr. A could probably give this talk as well as I could here, but I will try and then you please feel free to add. Obviously, we've heard of the microbiome, we've heard of the microbiome that exists in our gut, maybe in our mouths, on our skin, and it turns out that we also have one in our vaginas. And it's just a fancy word for a community of bacteria and fungi that live in or on a certain part of the body.
And it turns out that the vaginal microbiome is actually playing a really interesting role in overall female health. But the only time today that we typically pay attention to it is when we have those symptoms. The symptoms of a yeast infection or bacterial vaginosis that drive us to the doctor's office. What's so interesting to me is that today, vaginal discomfort is actually a leading reason that women seek health care advice in the United States — you probably know this very well, Dr. A — it's the number one type of OBGYN visit. Thirty percent of women at any given time have BV, which is just one of the many infections you can have.
So it's this, frankly, causing a lot of really frustrating conditions for women. And unfortunately, when we go to the doctor, we are more likely to be misdiagnosed than correctly diagnosed. And we are more likely not to get better and to have our infections come back than we are to get better.
So you have the way that the vaginal microbiome is playing this role in kind of our day-to-day lives as patients and kind of a big part of the healthcare system as well. But what's so interesting about the vaginal microbiome is also the role that it's playing in our overall health outcomes. And of course, as I will say a hundred times, all of this could be better researched.
There could be way bigger studies using way better technology to answer these questions. But our current understanding seems to hypothesize that the vaginal microbiome is providing some type of immune barrier for the rest of the reproductive system. And what we see is that when the vaginal microbiome starts to break down, not only do we experience these symptoms and infections that drive us to the doctor's office, but what's actually happened is that we've lost these protective bacteria.
Maybe you've heard of Lactobacilli in the context of gut health or vaginal health. And what we see is that bacteria like Lactobacilli, what they're actually doing is producing lactic acid and hydrogen peroxide, and they're taking up space on the vaginal wall so that when pathogens get into your vagina — because remember, the vagina is essentially an open gateway from the outside world to your reproductive system — those microbes can't survive or thrive because the environment is simply too acidic, there's no space for them. And in that way, the vaginal microbiome is actually keeping those pathogens out of the reproductive system. But when it breaks down, what you start to see is that those pathogens are able to replicate.
I always say, God forbid you have sex with someone new or your period lasts a few days longer, or you sit in your swimsuit too long. All of those things can elevate your vaginal pH, allowing those pathogenic microbes to replicate. And that's when we go to the doctor with these symptoms and infections.
But what research is starting to show is that in those moments, we are also at much higher risk for everything from IVF failure to preterm birth, to cervical cancer progression, to STI acquisition. Because we've actually now allowed those pathogens to travel up the reproductive tract and cause inflammation.
Mary Alice: So, Dr. A, can I ask you a medical question? So, you're born, I'm born a female, and everything's perfect about you. Your vagina's perfect, your gut's perfect. What changes?
Dr. A: But your vagina always has bacteria and yeast together, even when you're born. So it's like a colonization. For example, I use Ureaplasma or Mycoplasma — patients see it on their culture and they start treating it with antibiotics. That's the worst thing you can do because sometimes the more antibiotics you take, the more you disrupt this lining. Yeast and bacteria are almost in equilibrium. When you treat one, the other one grows. When you treat the bacteria, yeast grows. And that's why, like she said, I have so many patients who come to my office and I don't even have time to see them. Sometimes they just come in, they self swab, and leave because, I mean, the calls are so frequent. And at the end of the day, you have to let your immune system, you know, fix a lot of these symptoms.
Most likely, your body will get rid of it. I have patients, Priyanka, who come to my office, they're anxious and depressed because of chronic yeast or chronic BV, but it becomes this vicious cycle. And the first thing I always tell them, I'm like, stop, just stop treating it.
You know, we all itch maybe a little bit. You might have a little bit of a discharge. You don't have to attack every time you see discharge on your underwear.
Mary Alice: How do you know if it's normal versus something that needs to be treated?
Priyanka: I think so often we as women are so bad at talking about our symptoms. We've been taught to normalize things that aren't normal, and we’re overreacting to things that maybe are normal. And I think so much of that goes back to just a lack of literacy that we have about things like our vaginal health. I don't think we learned anything you just said when we were in school.
Mary Alice: Nobody told us that. Literally. What you just said, nobody told us that. Sometimes just leave it alone. It's the same thing about your stomach. It used to be that you ate antibiotics like candy, and now we're like, no, that's going to totally disrupt your gut. And it's probably disrupting your vagina microbiome.
Dr. A: No, a hundred percent it is.
Priyanka: I always say if you take an antibiotic for an eye infection, it's still going to affect your vaginal health. The antibiotic doesn't know that you're taking it for your eye infection. We've seen now 50,000 of these women who are just exactly the way you described. It's so frustrating. And I think part of what makes it so hard is that you don't actually have the data to know when things are normal and when they're not normal. And so much of what we see from Evvy patients is actually the fact that you can take the swab yourself, learn yourself. This is what's normal. My vaginal microbiome is actually in a good place. I don't need to be stressed. And when I feel my discharge changing throughout my cycle, that's actually normal. Versus when I take an Evvy test and it's actually a problem. Now I actually start to learn when something is problematic and when I actually can let it go.
I think so much of what we're trying to do is give women that information on their own bodies so that they can advocate for themselves when they need to. And so that they can also relax when they don't need to be stressed about it.
Mary Alice: So walk us through the test and what happens. I know you guys also have telehealth if they need to talk to a doctor. Walk me through the process.
Priyanka: Well, I wish everyone could have Dr. A at their fingertips, but unfortunately that isn't the case for so, so many women. And so part of what we're so focused on is increasing access to really high-quality vaginal health care.
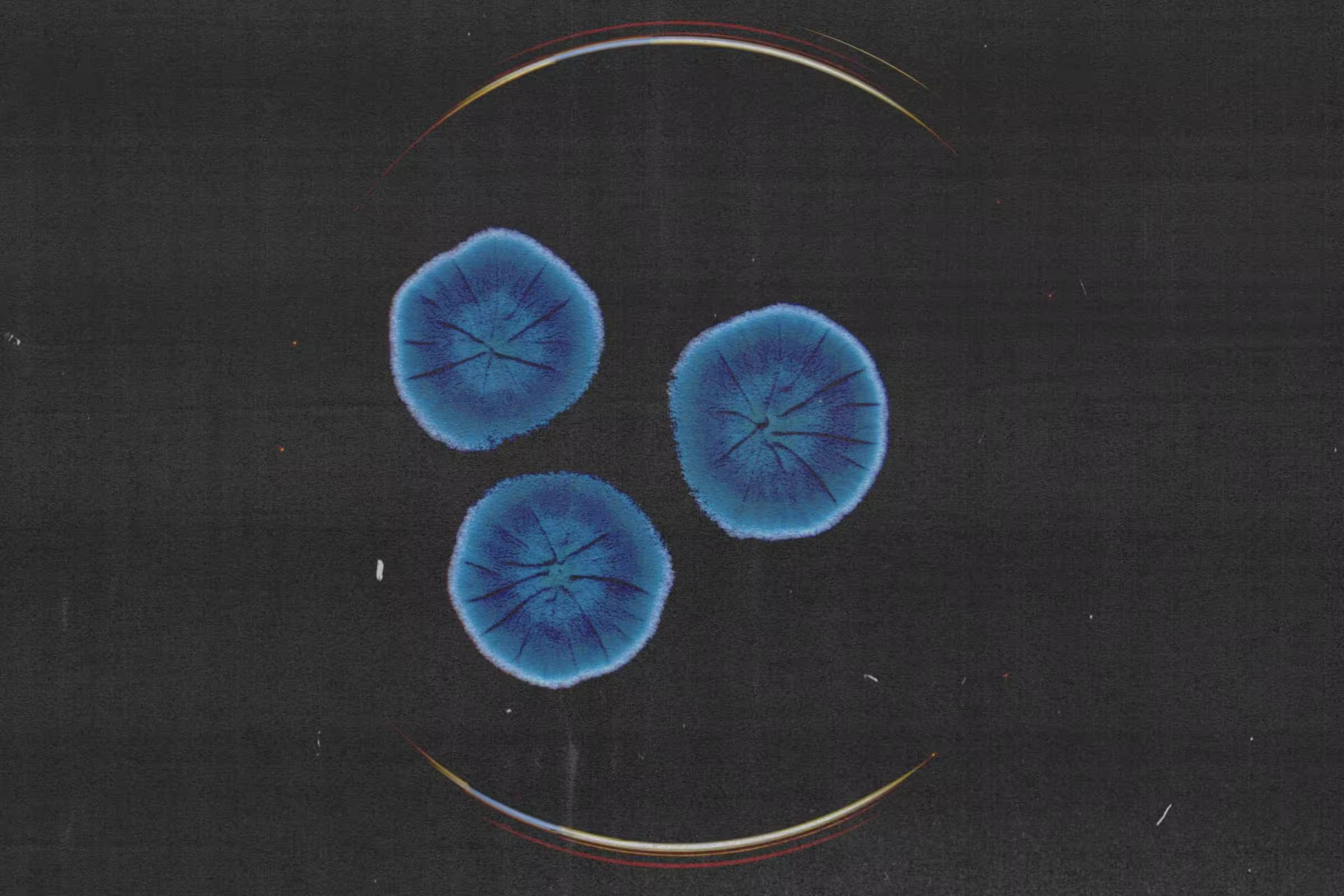
We have patients who come to us who, you know, are in the population we described — recurrent symptoms, recurrent infections. We have patients who come to us who are trying to get pregnant or who are in menopause experiencing new vaginal symptoms. People who come to us to proactively take care of their microbiome. So many different types of people going through this flow, but what they're able to do is go to Evvy, order a vaginal health test, it's a self-swab that you do at home. I always joke it's easier than putting in a tampon. You mail it back to our lab, And what we're able to do is whole genome metagenomic sequencing on that sample.
And you've probably seen this time and time again, Dr. A. When we do testing today, we're doing a culture. We're looking under the microscope. We're smelling the swab. We're maybe doing a PCR test for one or two things. But at the end of the day, we're missing so much information about what's actually going on in that patient's microbiome. Maybe there actually is a pathogen that's present that's not on the standard panel. And we see that all the time. Or maybe actually their vaginal microbiome is dominated by healthy bacteria and what they're experiencing is irritation of the vaginal wall that has nothing to do with the microbiome. And so antibiotics aren't going to help that. And so we are able to look for all bacteria and fungi that are present in the vaginal microbiome.
And then really, our goal is to educate patients. So we take all of that information, we combine it with the information about a patient's symptoms, their health history, and we produce a really amazing educational experience for people to learn about their vaginal health. How are the microbes in your vagina related to the symptoms you have or not? How are they related to your health goals around fertility or pregnancy? How might they be related to the change in hormones that you're experiencing in menopause? And then we provide a step-by-step plan of next steps, so things to talk to your doctor about if there are pathogens present, and we also link to the research so that the everyday doctor can see for this specific patient what is the most up-to-date knowledge about what's going on for them.
And then if the patient doesn't have their own doctor, we are able to connect them to a provider in all 50 states who's then able to help them decide what to do next, if treatment is necessary. One of the things we care a lot about is not just throwing antibiotics at the problem. As you said, you've probably seen many of these companies, but on the internet now people can essentially just order vaginal antibiotics. And we're actually reminding them of the importance of the healthy bacteria. And that's actually the goal is rebuilding the good bacteria, not just taking more antibiotics. So we're able to help put them on a plan that can include treatment if it's necessary, but also lifestyle changes, helping people understand the role of sex and their vaginal health or condoms, um, understanding the role of different medications.
Our patients are able to kind of learn what's going on, get help through Evvy and then take proactive care of their vaginal health, right? So instead of waiting until. We have, you know, a full-blown infection, we can actually stay on top of things much earlier than that.
Dr. A: Let me ask you a question. When we talk about vaginal infection, it could be bacteria, it could be yeast, it could be viral, it could be parasitic (like trichomoniasis). Do you check for HPV? Do you check for herpes? Do you check for trich? What do you check for?
Priyanka: Great question. We look for all bacteria and fungi that have ever been isolated from the urogenital tract. And then we have an additional panel that can be run on the same swab that looks for four STIs, including trich, Mycoplasma genitalium, chlamydia, and gonorrhea. We don't test for HPV or herpes because a vaginal swab has not been clinically shown to be the best way to test for those two conditions. We encourage patients who do want to test for those two things to go to their doctor to do the gold standard test.
Mary Alice: Well, that's so great because sometimes these young girls, they're nervous and some of them won't go to the doctor because of the stigma and the shame. If they have that ability to do that at home, that's really incredible.
Priyanka: And we see almost over half of our patients now add on the STI test and what's been so interesting to see is that the majority of them tell us they've actually never done an STI test before. So we're also trying to increase access to that type of proactive testing, which can be done from home and on your own terms receiving treatment when you need it. But without kind of having the inconvenience or the shame of going to the doctor.
Dr. A: I can speak as a gynecologist, anyone 24 and under who are sexually active, I pretty much force them to do annual STD tests. If they have a new partner, we do it. If they start having a relationship with another guy, sometimes I bring the guy, I don't have to see him, but he comes to my office and we do full panel STD. You always have to protect yourself. But I also want to go back to the discharge because a lot of people confuse bladder infection, vaginal infection. There's so much lack of knowledge, so I just want to quickly review it.
The two most common infections in the vagina are either bacteria or yeast. And if you're at home with bacterial infection, patients usually have some creamy discharge. They get mild itching. They can have severe itching, but the itching is usually not as bad as a yeast infection. And they usually complain of a foul-smelling fishy odor, even when they urinate. So sometimes they go to pee and they smell an odor and they worry that it's coming from the bladder, but it's coming from the vagina. And when you sit to urinate, that's when you smell it. So that's a bacterial infection. Yeast infections give you this cottage cheese, thick discharge and it's usually associated with a lot of itching. And usually, it might smell, but you don't have that foul odor with it. So if you have white cottage cheese discharge and it's really itchy, it's most likely yeast.
Usually, we see yeast infections in anxious patients, patients who've been very stressed, and patients who take antibiotics. For bacterial infections, on the other hand, when patients have unprotected sex, the semen is very basic and it changes the pH of the vagina so then the bacteria grow. Patients come and they're like, my partner gave me something. It's not like the partner gave him something, the partner's semen changed the pH of the vagina which made it a better environment for the bacteria that’s in the vagina to grow. For bacterial infections, we have to sometimes treat with antibiotics when it's really bad. We have vaginal antibiotics in cases for patients when they don't want to do the vaginal creams. For a yeast infection, we have the pill, we have the cream. I like using boric acid because boric acid helps bring the pH back to normal without having to blast patients with so many antibiotics.
Mary Alice: Do you put boric acid inside the vagina?
Dr. A: In the vagina. I prescribe 600 milligrams of boric acid, which you can't get online. It has to be a prescription and it's compounded. 600 milligrams every night for seven nights, and then twice a week for three weeks. And a lot of patients with recurrent BV or with recurrent yeast infections start feeling better because you're bringing the pH back to normal and you're letting their vagina heal and the good bacteria to give them that protection again.
Sometimes in severe cases, I continue with the boric acid, but at a lower dose after a month, I give him 50 milligrams twice a week for three months as a suppression to keep the pH normal. Sometimes in severe cases, we have to suppress yeast infection with weekly Diflucan for six months. And these are usually patients who are just so anxious and you just, and they've taken years of antibiotics, this and that, and it's, you really have to suppress them for six months to get everything back to normal. And with that Diflucan suppression once a week, I also give them the boric acid.
In case of bacterial vaginosis with severe recurrent cases, you have to treat the partner to make sure it’s not going back and forth, and then you can suppress it with vaginal antibiotics twice a week for three to six months, which I don't like doing. So I always, always, always go to boric acid first. And only if that fails and my patients are just miserable, and they have to have a positive culture. Sometimes we do a culture and it says low BV. You have no reason to treat that low BV. You don't need to treat vaginal infections if patients are asymptomatic.
Mary Alice: So it's all about the symptoms.
Dr. A: For example, we do pap smears, and sometimes the pap smear can pick up yeast. You call the patient. The patient has no symptoms. Let it be. Okay. You don't have to constantly treat everything.
Priyanka: I love everything you just said and exactly what you do is what we try to provide to patients around the country who don't have access to you, that very similar set of protocols. And I think one of the problems is with the actual testing itself, right? Because here's the thing, if you're doing a culture, you're just seeing, is this microbe present in the vagina?
And as you said, most microbes are present in the vagina, even ones that are pathogenic, but that doesn't mean that they are causing an infection. Because what you'll see is that if you have 1% Gardnerella, then that actually probably is totally fine. Versus if you're 99% Gardnerella, that's when we start to have an issue because now you're lacking those protective microbes that keep the pH low and do everything that you just described.
I think the challenge today is that we don't have the tools to separate between those two situations. And that's often why we depend on symptoms. We have patients with up to 30% disruptive bacteria who have no symptoms at all. So to your point, having the microbes present there is actually not a sign of infection. Many of them are actually just natural inhabitants of the vagina.
Mary Alice: If you take antibiotics, you take a probiotic for your stomach. Do you take one for the vagina?
Priyanka: Great question. Again, research could be much better on all of these topics. But currently, the research shows that oral probiotics are not the best way to change the vaginal microbiome.
When our providers prescribe vaginal probiotics, they're typically prescribing a vaginal suppository format versus an oral format. One thing I will add is that there have been studies that show that taking a probiotic for your gut health does, over time also improve your vaginal health. And there are a few hypotheses around your immune system being stronger, better modulation of estrogen, both of which then translate to better vaginal health. But we're not seeing that the strains that you take in an oral probiotic are colonizing the vagina.
Mary Alice: So Priyanka, because you have now this new data set of 50,000 women, are there things that you've learned that are sort of cutting edge that you want to share today?
Priyanka: Yes, definitely. One of the main things that we wanted to do was further the research in this area so that we could better understand these conditions that are affecting so many women today. But then also that we could actually understand the mechanisms of action for how the vaginal microbiome is playing a role in women's health conditions so that we can start to leverage it to potentially be more proactive around these other outcomes.
We very excitingly now have the world's largest data set ever on the vaginal microbiome. When people sign up for Evvy, one of the first things that we ask is if they're open to their data being included in research, obviously anonymized. And actually 98% of our patients to date have actively consented to research. We have so many women who write to us saying, what else can I tell you so that my daughter or my sister never has to deal with these same problems again. I really believe that women are going to be the ones who improve women's health. We are the ones who are the most motivated for these problems to change.
And because of that incredible community that's been built around this, we have really interesting and robust data on what the vaginal microbiome looks like in a very, very diverse population across everything you could imagine, race, ethnicity, age, demographics, location, history of infections, other diagnoses. And what we're starting to see is that what we consider bacterial vaginosis or vaginitis at a high level is actually many, many different things. We see a variety of different molecular signatures that are clustering around different symptom profiles or around a patient who is pregnant versus postpartum versus in menopause, versus on a certain birth control. All of those things are playing a role in that specific patient's vaginal health. And so what our providers are starting to do is instead of just looking at bacterial vaginosis, they're looking at what we've now stratified into over 80 different permutations of what the vaginal microbiome can look like in these different populations.
And when you're looking at the vaginal microbiome at that much more specific level, you're then able to be much more precise with what's most likely to help that patient. So again, are they 95% healthy bacteria? In that case, we probably don't want to use a vaginal antibiotic that's likely to wipe out those good bacteria.
And even for the different types of pathogens in the vagina, the microbes are more or less likely to be susceptible to those different antibiotics. So, we’re allowing patients to have much more personalized care, and I always say, precision health starts with data. So, we're very much trying to build the data to enable that precision care.
Dr. A: I have a question. Talk to us about birth control pills, progesterone IUDs, and copper IUDs affecting the vaginal microbiome.
Priyanka: That's such a good question. I actually am so curious to do this research on our own data set because we are looking at the types of birth control that our patients are on, and obviously the studies that have been done are all tiny.
That said, we don't seem to fully understand the relationship of the hormonal birth controls on the vaginal microbiome. We see differing impacts. Some patients have more infections. Some patients have fewer infections. So, that has not been answered, but what the studies have shown is that the copper IUD seems to be more likely to be associated with more infections for patients.
And there are two current hypotheses for why that is. One is that the device itself is allowing bacteria to grow on it and create biofilms and kind of get trapped there and are hard to treat. And then the second is that the copper IUD specifically is typically associated with heavier periods, so there’s a lot more menstrual blood. As you discussed with semen, a very similar phenomenon happens with menstrual blood, where menstrual blood is more basic than the vaginal microbiome. And so what we see is that when it's present for a longer period of time in that woman's cycle, pathogens in the vaginal microbiome are more likely to grow.
Those are the only associations that have been shown in the literature so far.
Mary Alice: Well, I've always wondered this. Every time I put a tampon in, I'm like, why isn't this giving me a lot of bacteria? That thing is sitting inside my vagina.
Dr. A: That's why you have to pull it out!
Mary Alice: But you know, sometimes you leave it in there for a little bit.
Dr. A: You shouldn't.
Mary Alice: How long should you leave a tampon in?
Dr. A: Eight hours.
Priyanka: No more than eight hours.
Dr. A: If you pull it and change it, you're fine. A lot of people change it within four or five hours, especially the first few days. The most important thing is not to leave it. The longer you leave it, the more likely you are for these bacteria to multiply and get you infected.
Mary Alice: And then I know the answer to this, but I want to hear you say it, Dr. A. douching.
Dr. A: It's not good.
Mary Alice: Tell everybody why.
Dr. A: You wipe off the lining that she's been talking about for the past 45 minutes. You disrupt that pH, you disrupt the lining. There's no reason to douche. You can use soap on the outside, but there's no reason to insert something and disrupt that lining.
Mary Alice: What happens when your estrogen drops in your vagina?
Dr. A: It's a nightmare, that’s what happens!
Priyanka: It is. I mean, it affects your vaginal health in so many ways. Doctor, I'll let you talk about the vaginal epithelial wall and the things that are not microbiome-related, but I can touch on the component that is related to the microbiome, which is that estrogen produces glycogen. And glycogen is actually one of the main food sources for the healthy microbes that live in the vagina.
So when that food source gets depleted, we see those healthy bacteria go down in count and we start to see higher rates of things like bacterial vaginosis, yeast infections, and recurrent UTIs. Because what often happens is the pathogenic bacteria has colonized the vagina, and then it's just traveling back over to the bladder, right, and consistently causing these infections.
So that's the role of estrogen in the microbiome, but Dr. A, there's a lot more to say.
Dr. A: I was going to say, one of the main issues is the dryness that comes with a lack of estrogen. You lose elasticity, you lose collagen, just like you do on the rest of your body on the skin. But specifically in the vagina — and speaking of recurrent UTIs — the urethra, which connects the outside to the bladder, has an elasticity with it. As it gets dry, the urethra, the outside of it gets dry and stiff. So it's more common for bacteria, especially during sex, or if you wipe yourself from back to front, you're more likely to get these bladder infections.
And that's why a lot of times when women after menopause complain of recurrent bladder infections, the first thing we do is treat their vagina with estrogen. I do the Mona Lisa laser or CO2 laser of the vagina, and that brings elasticity and flow back to the outside of the urethra and to the vaginal walls and it reduces the risk of these infections.
Mary Alice: So, another question, asking for a friend. If you're taking a patch, or you're taking progesterone, can you still take vaginal estrogen?
Dr. A: Absolutely. So, some people when they use systemic estrogen, get relief vaginally because it's systemic. But a lot of times we have to treat it locally. So you can do the estrogen patches and still do the vaginal estradiol, which helps a lot.
Guys, I want to add one more thing because you know, I love endometriosis — I mean, I don't, I hate endometriosis, but it's my passion in life, I hate it with every cell in my body — but endometriosis patients, here's a typical. patient, right? They have these bladder symptoms. So a lot of times these endometriosis implants that sit on the bladder, I removed one yesterday, like extensive lesions on the surface of her bladder. These patients constantly go to their gynecologist or their family doctor with UTI symptoms or bladder symptoms. Irritation, frequency, urgency. What does the doctor do? Write a prescription for antibiotics. And what did they do? These patients get treated six, seven times a year with systemic antibiotics. It's tragic. And as I'm listening to them, I'm like, this is endometriosis bladder discomfort. It has nothing to do with UTI. And I always tell them, I'm like, show me a positive culture. They're like, no, no, no, I had a positive culture. I'm like, I want to see your positive culture.
Mary Alice: So how do you, how can you tell the difference?
Dr. A: Listening to your patient, if the patient's having symptoms of frequency, urgency, bladder irritation, pelvic pain that comes with painful periods and painful sex, and everything else. It's most likely not a UTI. But always, always, always send a culture before you start taking that antibiotic. You must do that.
Priyanka: I feel so strongly about this. This is what I was saying. And you know, when we think about vaginal health, I think there was a study that showed that 66% of people who think they have a yeast infection actually have something else. They're not going to their doctor. They're buying over-the-counter products. And now, because there are so many services online where you can just essentially order vaginal antibiotics, patients are taking vaginal antibiotics over and over and over again. And that's why at Evvy, even though there's a lot of money to be made in prescribing those online, we require test results that show us that there's actually an imbalance of bacteria for us to prescribe any of those. And we find that most patients are actually mad at us for that because they're like, well, my doctor will just prescribe it to me if I call them. And I'm like, well, we care too much about your vaginal microbiome to do that to you.
Dr. A: The other thing is postmenopause vaginal itching. If you're postmenopausal and you have itching, chances are you have vaginal dryness and not a yeast infection. What do these patients do? Monistat, Monistat, Monistat. And they're like, I'm not getting better, I have recurring yeast infection. No, you don't. You have vaginal dryness.
Mary Alice: So we launched Ovii because in the same way that you did with Evvy, we want to take all of the expertise that Dr. A has had treating PCOS and give them a real solution that they can do in their own home in a similar way. How does insulin resistance, which happens so much with PCOS patients, affect the microbiome?
Dr. A: Such a good question!
Mary Alice: See, I'm actually good at my job!
Priyanka: I mean, my answer to everything in women's health, especially vaginal health, is why has nobody researched these things? We obviously now have the data. We want to do this research. I wish our team could be five times the size and that we could get all the money from the government to help us do this research. But unfortunately, that is not the world we live in. That said, there are studies on actually both endometriosis and PCOS and the vaginal microbiome. Of course, we don't have any definitive answers yet, but what we are starting to see is that patients with, and I'll start with PCOS because that's what you asked, patients with PCOS who tend to have hormone imbalances also are more likely to have vaginal infections.
What we see is that research has pointed to kind of two things. One, those hormone imbalances increase the risk of vaginal infections, and two, that there might actually be interesting biomarkers in the vaginal microbiome for patients with PCOS. So that's something we're hoping to look into because obviously we would love to have better diagnostics for PCOS that can be done at home for patients.
Similarly for endometriosis, there's actually, again, two interesting things that research is starting to show with the vaginal microbiome. One is similarly around biomarkers. There's a really interesting set of research showing that we could potentially find molecular signatures for endometriosis in the vagina.
And obviously we would love to have something as non-invasive as an at-home swab assist with that diagnosis, which, as you know, Dr. A, usually takes far, far too long, and requires surgery. Um, but also it seems like there may actually be a bacterial component to the progression of endometriosis. And again, not well understood yet, but we are very curious to continue looking at if the pathogens in the vaginal canal could be playing a role in that progression.
Mary Alice: It's so interesting. But before we close, because you are now an expert on the vagina, give us five tips that you want every woman to know about her vagina or something that she should be doing to keep her microbiome healthy and amazing.
Priyanka: Yes. Love that. One is definitely go to your doctor or get a test before you assume that you know what's going on down there. I think, unfortunately, we have not been well educated. We have not had the tools to do this self-diagnosis at home. And I think that it's leading to more problems in vaginal health rather than actually solving them. Two is to pay attention to how you feel. I think, unfortunately, so many patients go to the doctor and they're told that they're fine when they're really not fine. And so I think I always say you're the expert on your own body. So you need to get the data. You need to become the expert on your body so that then you can advocate for yourself in those settings.
Unfortunately, not everyone has Dr. A on the other side, and so remember that you have to advocate for yourself to bring the data to bring the research to really make sure you're getting the best possible health care for yourself. Um, three is to remember that sex plays a huge role, and whether it's oral sex, it's penetrative sex, sex is the largest trigger of vaginal infections and not all vaginal symptoms are STIs. So remember that the introduction of semen into the microbiome, even the oral microbiome and the vaginal microbiome, all of these things can introduce new bacteria, change the pH, which then can affect your vaginal health.
And those are things to pay attention to because we don't want to leave true symptomatic infections untreated and unresolved. Um, and then lastly, I hope that people talk about this, right? I think it's amazing that we're sitting here talking about vaginal discharge and vaginal odor. These are things that affect one in three women at any given time. And it's so unfortunate that we think that they are shameful, that we don't want to talk about them, and that we feel alone. So I'm so grateful for the amazing platform that you all are providing so that everyone who is dealing with this doesn't feel alone in their journeys.
Dr. A: You're amazing!
Mary Alice: And again, I appreciate all that you are doing to shine a light on the inequality in women's health. Dr. A and I talk about this all the time. People said, I wish I had a doctor like Dr. A. and she says, what I want to do and why we started the podcast and why you started Evvy was we want to give you the tools. We want to give you the knowledge to be your own health advocate and take that to your own doctor. Or sometimes in the case of Evvy, maybe you don't even need to go see your doctor. Maybe it's something that you can handle yourself. So I really appreciate everything you're doing.
Priyanka: I mean, amen. I think that what we need in this space is people to innovate. We need people to come up with better diagnostics, with better treatments. It is just unacceptable that in 2024 we as women don't have tools to get the right diagnoses, to get the right treatments, to do the things that we want to do. And I think that it's just, I'm so grateful for the work that you're doing. I think about 10% of Evvy patients have PCOS and I can tell you that there are so few solutions for them so I'm so grateful for the work that you're doing and we can't wait to share it with our community as well.
Mary Alice: Amazing, amazing. Thank you.
Priyanka: Thank you so much!
Dr. A: Take care.
Mary Alice: Take care, Priyanka.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.